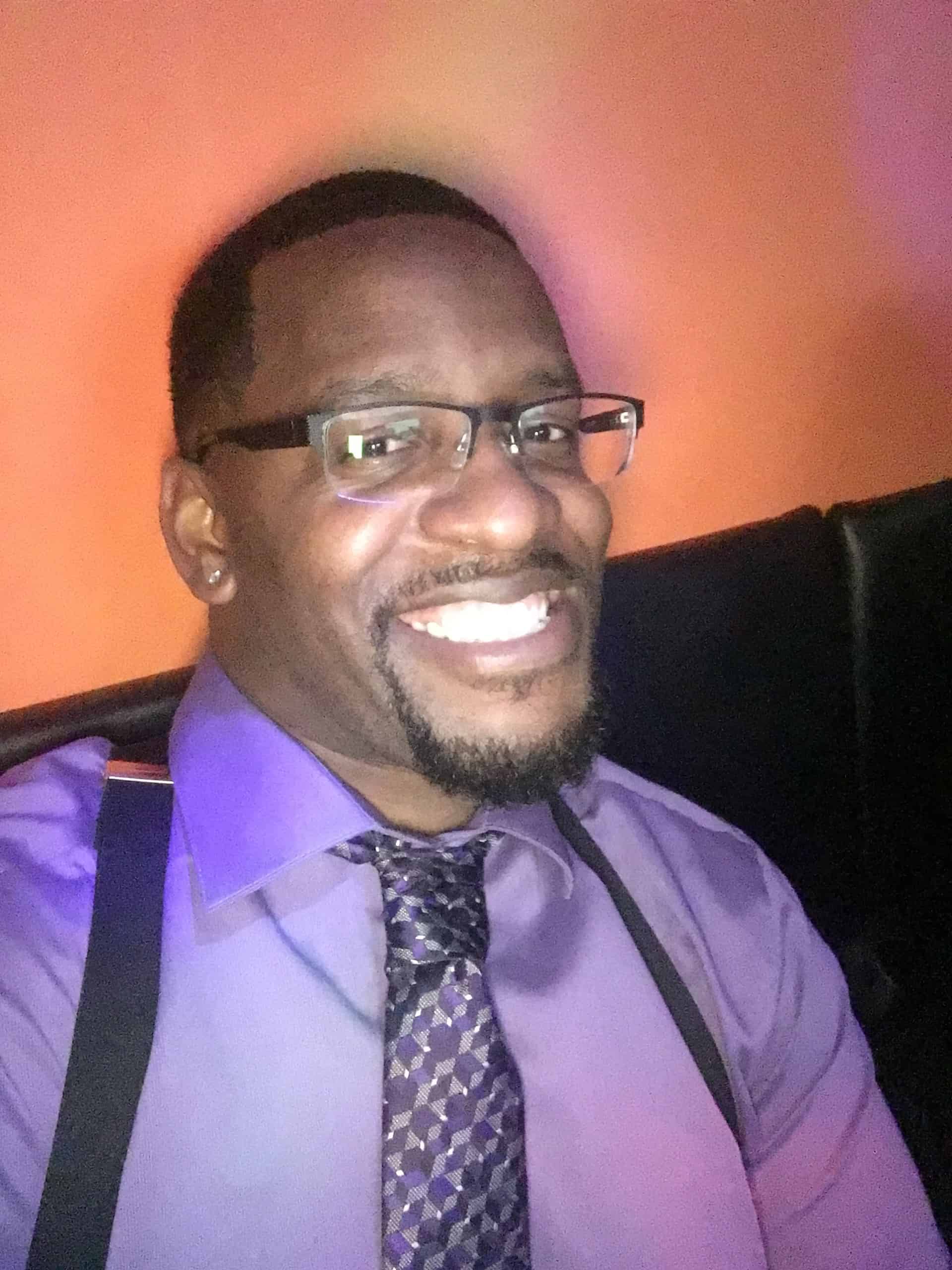
Respiratory Therapist on the front lines of pandemic in hard-hit New York
 On his way home after every 12-hour shift, Eric Wise walks by the long-refrigerated truck his Brooklyn hospital must use to house the escalating number of deceased Covid-19 victims. “Every day I’m walking by a truck with all the bodies I’ve just bagged up,” says Eric. “There are days so many died. You have to psych yourself up because this, right here, is something that’s never been seen before.”
On his way home after every 12-hour shift, Eric Wise walks by the long-refrigerated truck his Brooklyn hospital must use to house the escalating number of deceased Covid-19 victims. “Every day I’m walking by a truck with all the bodies I’ve just bagged up,” says Eric. “There are days so many died. You have to psych yourself up because this, right here, is something that’s never been seen before.”
For several weeks Eric has been a ‘stranger in a strange land’, as one of many medical ‘travelers’ who leaves everything familiar to join the frontline fight against the coronavirus. As a Registered Respiratory Therapist his specialty was in great demand for a disease that traumatically impacts the body’s cardio-pulmonary system.
Why would anyone sign up for the often futile and potentially high-risk exposure that provision of medical care in this arena invites? “I said ‘yes’ based on the merit of doing whatever I can do to help anyone in a crisis,” he says.
The timing was right for Eric, who had just completed a 14-month hospital contract in Virginia his ‘traveler company’ had assigned him. Having just graduated from San Joaquin Valley College’s Respiratory Therapy program before signing on with this placement agency, Eric appreciated all the hands-on experience. “I had just graduated and was eager to get my feet wet in the medical field,” he explains.
But this 14-week assignment that would take him to the pandemic’s epicenter was way beyond any skill proficiency he might have sought. “There’s no better experience than what I’ve had with this Covid,” says Eric. He brought all his developing expertise to the forefront and found a balance of professionalism and compassion he may not have previously realized.
Eric also found a way to prove himself and set an example for others who might be watching, including his 8-year old son, Ethan, who lives in another state with his mom. “You have to pave the way for the next generation, and this is an example for my son, that he can do anything he wants to do. You just have to go get it.”
Eric joined the Brooklyn hospital’s medical team as Covid was in full swing. His 12-hour days sometimes stretched to 6-7 days in a row, and a constant shortage of PPE (Personal Protective Equipment) was a great concern. “We had to wear the same gown and mask longer that we should have,” says Eric. “To do the job we’ve done with the limited resources we’ve had is remarkable.” Over time supply chains were much improved.
The hospital became a world unto itself. Once staff entered the building and put on protective gear, there was no leaving until they were done for the day.
There was no way to anticipate the severity with which Covid struck the human body or how quickly it could become life-threatening. “Most people who came in needed ventilator treatment, many a lot sooner than they got it,” says Eric. “A lot didn’t make it because they came in too late and were already so severe that we basically provided comfort care before their inevitable demise.”
Others came to the hospital “just not feeling right”. Covid carriers can be asymptomatic. “They can be talking, maybe feel a little lightheaded, dizzy, then all of a sudden, they tank,” says Eric. “They’re taking deeper breaths, air-hungry, blood pressure goes down and they start dropping. If there’s a fast heart rate – that little point right there – forget bypass and go to the ventilator.”
Eric estimates that at Covid’s peak 90% of patients at their hospital lost their lives, regardless of medical intervention. “If you have any other health conditions (COPD, high blood pressure, diabetes, autoimmune disease, i.e.,) it inflames this virus and makes it even more deadly.”
The Intensive Care Unit (ICU) is Eric’s primary workstation, though he is called to another areas every day. “I’m in the psych ward, med/surge unit; You’ve got to help out where you can.”
Life’s breath can be compromised, taken away at any moment.
“The most important thing we do is ventilator management; intubating someone and putting them on a ventilator,” he says. Ventilators are mechanical devices that breathe for the body to which it is attached. “Our goal is to let the patient get stronger, then use less of the vent while the patient does more of the breathing work,” says Eric. “We adjust pressures and volume and use less sedation when they start to recover.”
Medical teams are in daily contact with patients’ families, giving them updates on their loved ones’ care. “As much as we’ve had very bad (outcomes), some patients have made the full 180 and are walking out,” says Eric. “They’ve miraculously made a turnaround, are shaking our hands and thanking us. We’ve seen the fruits of our labor.”
Too often it goes the other way and patients who are clearly in severe decline are given only ‘comfort care’. Family members are called, and one-sided Facetime goodbyes are arranged. “We make the patient very presentable, hold the zoom or iPad where family can see them, and they know they’re never going to see the patient again.” There is no possibility of verbal exchange. Families talk of past times, shared memories and forever love. “They will remember their loved one in a comfortable state, no pain,” says Eric. “My hope, my feeling at that moment is that my patient is saying, ‘I’ve made peace in my life; I’m ready to talk to Jesus.’”
Days like these are hard to set aside. Eric walks to his temporary apartment and the bits of refuge and distraction he can find. “It’s pretty much working out and Netflix,” he admits. “I have a heavy table and a little bench to do push-ups and sit-ups. It’s pretty much all calisthenics, all core muscle workouts. It relieves some of the stress, for sure.”
Eric is stressed, but not overwhelmed. “SJVC (Respiratory Therapy program) did prepare me; all the hurdles and obstacles you had to get through to meet deadlines, to complete tasks when you’re tired, to be where you’re supposed to be on time. We were held accountable. Leadership set that foundation and that standard. And having all that for your patients is important from Day One.”
It was Eric’s dad, Eric senior, who scouted the Respiratory Therapy program at SJVC’s Visalia, CA campus. “Charmaine Wojitas, the Admissions Representative first talked with my dad,” says Eric. “Based on Dad’s experience with her and his advice, I’d already committed when I picked up the phone to talk with her.” His intuition was well founded.
“The leadership there want nothing but for you to succeed,” Eric reflects. “They take pride in developing the students into young medical professionals.”
Eric was both working and going to school full-time when he reached the last term in his program. “We all kind of had ‘senioritis’ and I was real weak in PFTs (Profusion Function Tests). He told me to ‘Be better’,” says Eric. “He challenged me to turn one of my biggest weaknesses into one of my strengths. If I hadn’t learned that, I wouldn’t have been able to advance in my testing and get my license and wouldn’t have been able to get to where I am now.”
Eric credits his mom (Cynthia) and dad (Eric) with a lot of what drives him. “I am the perfect blend of my mother and father. All of my compassion, mercy and empathy comes from my mom. From my dad it’s accountability, responsibility and no excuse – just handle business.”
All those values come together for one primary purpose. “Always first is my son,” says Eric. “To be an example for him; to give him the blueprint for where he wants to go in life and how to get there.”
Eric has enough inspiration to go around and, like Johnny Appleseed, he is planting those seeds generously.
You might also like
More stories about
Request Information
All fields using an asterik (*) are required.


