SJVC Respiratory Therapy Graduate Travels to New York to Help Treat Covid-19 Patients
 Jenn Anderson, a graduate from the Respiratory Therapy program at SJVC Rancho Cordova, has long had the desire to help others. She began her career in the medical field as a hospital phlebotomist, and when her cousin was diagnosed with lung cancer in 2015, she became interested in lung disease and how to treat it.
Jenn Anderson, a graduate from the Respiratory Therapy program at SJVC Rancho Cordova, has long had the desire to help others. She began her career in the medical field as a hospital phlebotomist, and when her cousin was diagnosed with lung cancer in 2015, she became interested in lung disease and how to treat it.
“I had so many questions,” Jenn remembers. “But attending codes and getting to draw blood, it just wasn’t enough for me. I wanted so badly to be on the side of helping to save a life. I wanted to be part of making that difference in someone’s life or their death.”
Today, Jenn is doing just that. She currently works in a 291-bed stroke center hospital in Bronxville, NY, where she has been since April, 2020 on humanitarian leave to complete a travel crisis position. Her permanent position, where she has been for the past seven years, is as a Respiratory Therapist at Marshal Hospital in Placerville, California. She is scheduled to fly back to California in June, 2020.
“I already felt pride in being a respiratory therapist,” she says, “but now our work is a little more recognized and praised. It’s humbling to be a healthcare worker during this uncertain time.”
Jenn graduated from the SJVC Respiratory Therapy program in October of 2018.
“I don’t think sitting in a classroom can completely prepare you for the field work you will be doing,” she explains, “But SJVC is very devoted to their students, and offers a high level of structure.” Jenn attended other Sacramento Vocational colleges before finding SJVC. “By far,” she says, “SJVC provided the most passion for student success, accountability, and professionalism.”
Jenn’s job as a Respiratory Therapist, simply put, is to make sure her patients are breathing.
“I use whatever modalities are needed to keep them breathing,” she explains. “That could range anywhere from a simple nebulized treatment (a method of administering breathing medications through an inhaled mist), O2 therapy, BiPAP, or intubation to mechanical ventilation.”
She had mixed emotions about going to New York, but ultimately knew it was where she needed to be.
“My heart was telling me this was something I had to do,” she said. “I have to use my knowledge, experience, and hard-earned RRT license to help where I am needed. In California, we are not seeing the pandemic anywhere close to the magnitude of how hard New York is seeing it. Californians have had time to prepare and determine what treatments are and are not working for COVID-19.”
Jenn is excited to be at her new job in New York.
“They’ve made it clear that having the extra help is definitely appreciated,” she says. “I’m mostly working in the ICU, taking care of five critically ill patients who are all receiving dialysis and mechanical ventilation.”
As for “typical” days on a job—there aren’t any when it comes to caring for patients with this virus.
“COVID-19 is somewhat mysterious,” Jenn says. “Every day is different than the last. We are, for the most part, providing normal critical care to these patients; however, we are trying new things, such as nitric oxide and different ventilator settings.”
Her new job has already taught her a great deal in a short period of time.
“I’ve been helping out with procedures I hadn’t done back home,” she explains. “Because many of these COVID-19 patients have been on mechanical ventilation for 2-3 weeks, they are receiving tracheotomies. I’ve had the privilege of assisting physicians with bedside tracheotomies and bronchoscopes, proning, tube exchanges, a lot of suctioning and arterial blood gas punctures or drawn through arterial lines. Also, I am by my patients’ sides as they receive pacemakers in the cath lab, or cat scans. I love all the new experiences and procedures, and I’m soaking up all the knowledge I am receiving here.”
Her position in New York differs from her position in California because most COVID-19 patients are not improving as quickly as patients without the virus.
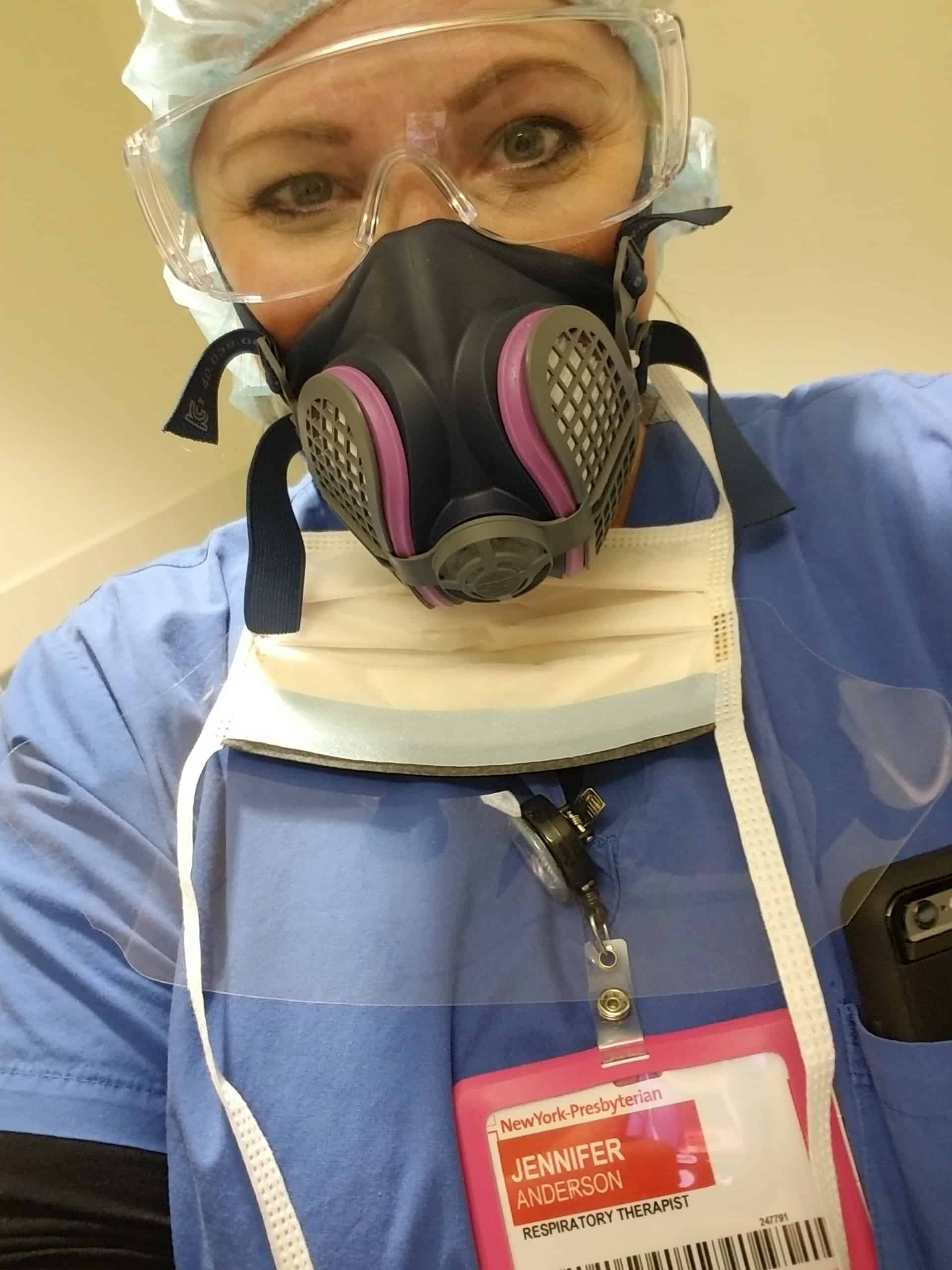
“I’m seeing patients for longer periods of time,” she says. “Having to wear an N95, goggles, and gowning up for every patient has been the biggest difference.”
For Jenn, this position offers a true, deep, and touching vantage point on life and death; she is with patients through every facet of their care—and for some, through their last breaths.
“I feel honored to be with and take care of these patients, some of them for their final days,” she says. “I will never take my freedom and health for granted. I may be the last person to see my patient alive, and the fact that they cannot have their family there with them during their final days is heartbreaking. I try my best to be compassionate and give them the best care.”
Want to Become a Respiratory Therapist?
Our free career guide tells you everything you need to know about respiratory therapy.
You might also like
More stories about
Request Information
All fields using an asterik (*) are required.


